Thank you for Subscribing to Medical Care Review Weekly Brief
- Home
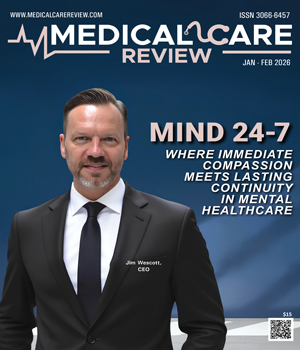
- January-February 2026
Medical Care Review: Specials Magazine
Access, compassion and immediacy define effective behavioral health care; yet, for many people, that combination remains out of reach. Most still end up in the emergency room. Designed for physical trauma, emergency rooms have become the default for mental-health crises, not because they are ideal, but because alternatives are scarce. They are rarely equipped to handle emotional or psychological emergencies, leaving patients waiting for hours in settings that heighten distress instead of easing it. Jim Wescott, CEO of MIND 24-7, saw those gaps firsthand. For more than twenty-five years, he worked as an emergency department nurse, watching families arrive in the middle of the night seeking help, only to leave hours later with little more than a prescription and a referral they would wait weeks to use. Those experiences shaped his vision for a better approach, one that treats behavioral health with the same urgency and respect as trauma care, while adding empathy, speed and seamless continuity. MIND 24-7 became his answer. It closes that gap by creating a system where no plea for help goes unheard and compassionate care is always within reach. Its walk-in crisis centers stay open around the clock, requiring no appointments and offering immediate support in private, calming spaces designed to assess and guide people through their most challenging moments. Each patient is evaluated within an hour in an environment built for emotional safety rather than medical urgency. “The hardest part for many people isn’t asking for help; it’s staying connected to it,” says Wescott. “Our model ensures that no one slips through the cracks once they leave our doors.” Each visit closes the loop, turning a moment of crisis into the first step toward continuous, connected care. Crisis stabilization, therapy, medication support and sub-acute treatment happen under one roof, with separate pathways for children, teens and adults. Case managers work beside clinicians to address the forces that often fuel a crisis due to unstable housing, food insecurity, family stress; so, recovery isn’t left to medication alone. After each visit, teams coordinate with hospitals, therapists and health plans to ensure the next step is already in place. Follow-up care feels guided, not left to chance.
Top Outpatient Mental Health Clinic in Minnesota 2026
For many, the first step toward care begins with the hope to find clarity, stability and support as they navigate their mental health recovery. IntegroRecovery Clinic meets them at that crucial juncture. Founders Alfredo Massa and Nicole Peluso launched the clinic in 2023 to provide outpatient mental health care for adults dealing with depression, anxiety, trauma, bipolar patterns, stress and perinatal mood challenges. The clinic is dedicated to addressing the root causes of these conditions, as most of them are deeply interconnected. “We help people who’ve been overlooked by fragmented systems, bringing all aspects of care together,” says Massa, MD, co-founder. A young woman with a complex clinical profile had cycled through this fragmented system for years. She had been in and out of treatment centers, often making progress with her depression, only to find her substance use and eating disorder resurfacing, a pattern commonly described as dual diagnosis. That is when she turned to IntegroRecovery Clinic for a more unified approach. Its clinicians integrated trauma-informed strategies and behavioral care into the treatment and worked with her former therapists and nutritionists to maintain continuity across all aspects of care. .
Bioidentical Hormone Replacement Service in New York
Away from the noise of big hospitals, a quiet awakening is taking root near Buffalo—where women navigating menopause, hormonal imbalances, and agerelated challenges are finally being heard, healed, and empowered. At the forefront is Chellino Health Nurse Practitioner, led by Tracy L. Chellino, MSN, ANP-BC, a board-certified Nurse Practitioner and nationally recognized expert in Bioidentical Hormone Replacement Therapy (BHRT). Founded on the belief that women deserve personalized, rootcause solutions—not symptommasking prescriptions—Chellino Health offers holistic, science-backed alternatives to conventional hormone care. While many clinics focus narrowly on pellet therapy, Chellino’s approach is more comprehensive, targeting the entire endocrine system, including thyroid function, testosterone, and more. Chellino’s journey is deeply personal. After a hysterectomy, she found little relief from traditional healthcare. “My primary care physician couldn’t help me. My endocrinologist couldn’t help me. I felt dismissed and helpless,” she recalls. That experience catalyzed her mission to change women’s healthcare. Determined to rewrite the narrative, Chellino pursued advanced training in BHRT and endocrinology—learning from the Hormone Health Institute and top practitioners in Texas. She holds a Master’s in Adult-Gerontology Primary Care from Daemen University, is board certified by the American Nurses Credentialing Center, and has earned a Master’s Certification in BHRT, hormone health, and Platelet Rich Plasma vaginal rejuvenation. With dual bachelor’s degrees in Nursing and Psychology—both earned summa cum laude—Chellino brings scientific depth and empathetic insight to her practice. Treating the Whole Hormonal System What sets Chellino Health apart is its root-cause, full-spectrum approach. Rather than masking symptoms with antidepressants or creams, Chellino focuses on restoring hormonal balance naturally. “Everything in your wellness begins with hormones. They are the foundation of health. When we rebuild that foundation, everything else improves—energy, mood, weight, sleep, relationships,” explains Chellino, founder and owner. Unlike most clinics that prioritize only estrogen and progesterone, Chellino highlights testosterone’s role in women’s vitality, strength, and emotional well-being.
Practitioner Insights

Destigmatizing Mental Health in Healthcare Space
Anne Mary K. Montero, Medical Director, Indiana University Health

Exploring the Journey of a Clinical Psychologist
Dr. Susan Rathmell, Licensed Clinical Psychologist & Owner, Upward Behavioral Health

Distraction in Digital Therapy
Beverly Wertheimer, PsyD, DMin, LCSW, Psychotherapist-Adolescent and Family Mental Health, Clinical Advisory Board Member, Daybreak Health
Integrated Care: Why It Works and What We've Learned
Teodoro Anderson Diaz, MS, MSW, LCSW, LADC, Vice President of Health & Wellness Center Outpatient Behavioral Healthcare, Wheeler Health

Driving Excellence in Patient
Patricia Punzalan, Sr. Director for Patient Care Services, Dignity Health

Automated Diabetes Management by Artificial Intelligence
Osama Hamdy, MD, Ph.D., FACE, Medical Director, Obesity Clinical Program, Joslin Diabetes Center

Tech Innovations to Improve Healthcare Processes
Audrey Neylon, System Director Mental Health & Addiction - Business Solutions, Fairview Health Services
IN FOCUS
Expanding Mental Health Access: The Walk-In Solution
Walk-in mental health care offers flexible access, operational benefits, and growth potential amid rising demand for timely psychological services.
Advancements Shaping Modern Outpatient Mental Health Care
Outpatient mental health care emphasizes accessible, community-based, and technology-enabled services, overcoming barriers while enhancing patient outcomes and system efficiency.
EDITORIAL
The New-Age Models Driving Mental Healthcare
This shift is shaping three key care categories across the U.S. Outpatient mental health clinics in Minnesota are supporting ongoing therapy and psychiatric treatment in structured, non-residential settings. On the other hand, top walk-in mental health care clinics are addressing immediate needs by offering same-day evaluations and short-term support without advance scheduling.
Alongside, bioidentical hormone replacement services in New York are gaining attention as part of a more integrated approach that recognizes the role hormonal balance plays in mood, cognition, and overall mental health.
This edition of Medical Care Review brings recent developments across these categories. It examines how leading providers are expanding access, integrating technology into clinical workflows, and refining mental healthcare models to meet evolving patient needs.
It features thought leadership articles from industry experts, including Beverly Wertheimer, psychotherapist specializing in adolescent and family mental health and a clinical advisory board member at Daybreak Health. She highlights how therapists tapping into “digital distractions” such as smartphones and social media can shape teens’ engagement in virtual therapy.
Teodoro Anderson Diaz, vice president of health & wellness center outpatient behavioral healthcare at Wheeler Health, traces how integrated care has evolved from a cost-driven concept into a collaborative, whole-person healthcare model.
We hope this edition helps you better understand the care models gaining traction across mental health services and supports your efforts to deliver care that meets patients’ evolving needs.